What Kerala's Rising Case Numbers Mean
High vaccination rates and good Covid-19 case management work in Kerala's favour, but its rising Covid-19 case numbers can't be taken lightly, especially with the festival season of Onam on the horizon, say public health experts V. Ramankutty and Rajeev Jayadevan
Mumbai: The state of Kerala in south-western India is now reporting roughly half the total daily new Covid-19 cases in India, even as we see the downswing of the second Covid-19 wave. This has raised several questions, including about why Kerala is seeing so many cases in proportion to other Indian states, what do these case numbers mean for the rest of Kerala, and about the ability of Kerala to cope with its caseload. More importantly, what does Kerala's experience portend, given that Covid-19 data from some other states are not as easily available in this quality? What is our understanding of the Covid-19 disease and its progression at this point between India's second wave and a possible third wave? How do we use Kerala's data to understand the potential behaviour of this disease going forward, as it could potentially spread to the rest of India?
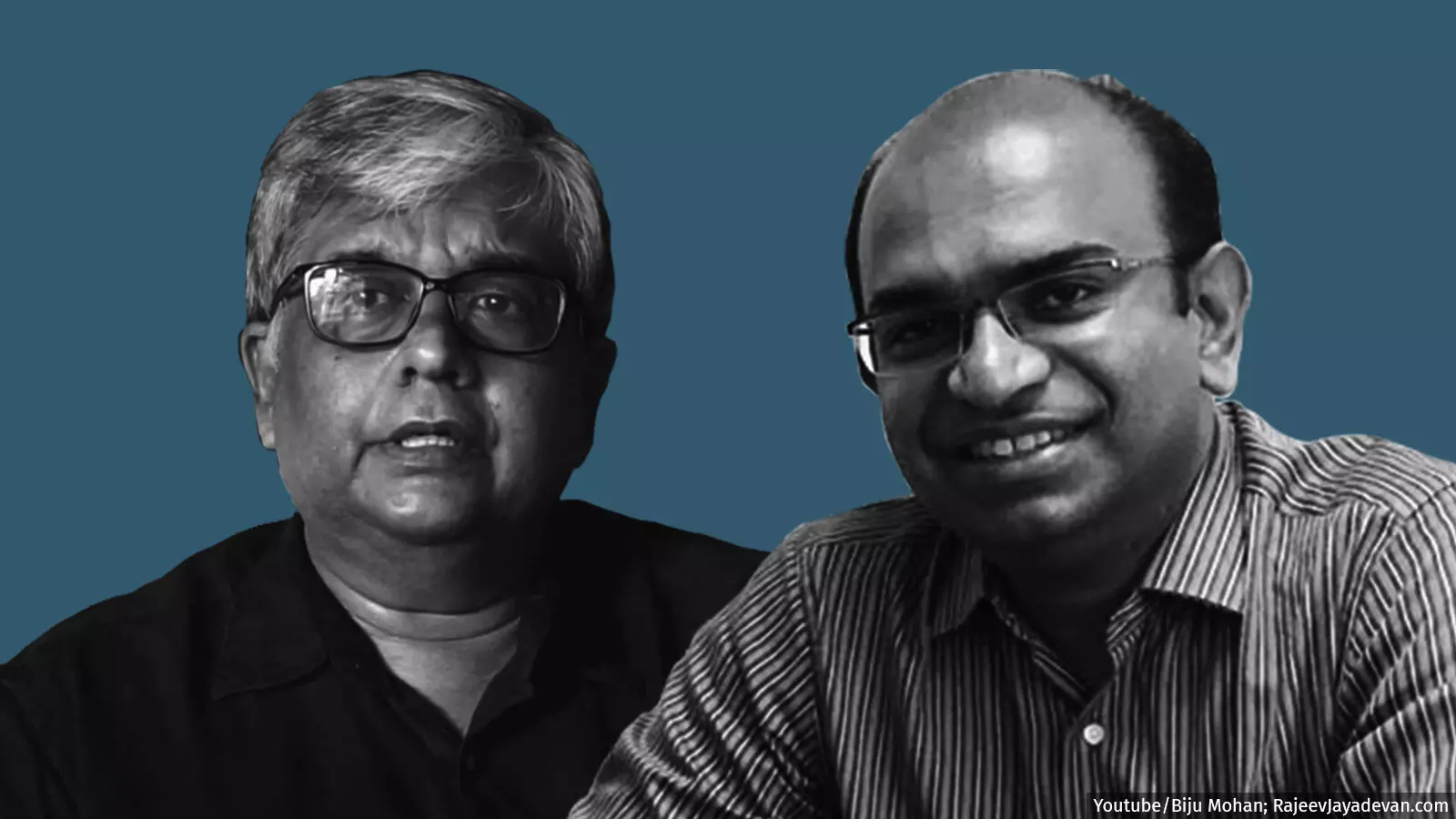
To answer these questions, we spoke with V. Ramankutty, epidemiologist and public health expert who holds a Master's in Public Health from Harvard University, and Rajeev Jayadevan, vice chairperson of the research cell of the Indian Medical Association. Both are based in Kerala.
Edited excerpts:
Dr Jayadevan, Kerala enjoys a very high degree of vaccination, at 23%, and is seeing about 24,000 cases per day at this point. What exactly is happening right now?
RJ: If you look at the British experience, at their past two Covid-19 waves, the answer to your question is very clear. They started vaccinating just before the previous wave and the apparent protection only occurred in the wave after. This means that the vaccinations we administer now will only show their true benefit in subsequent waves. As of now, there is an active spread of the disease in the community in Kerala, and it is happening within people's homes. But most of these people are not getting sick; thus the hospitals are not overloaded, so the vaccination effect is showing.
Over the last two or three weeks, there has been a slight increase in hospital admissions in Kerala, which is largely regional. For instance, I was discussing this during our regular Tuesday meetings which we have been having for the last year-and-a-half, where we keep stock of what is happening all around Kerala. From Ernakulam district, I can say there's a slight uptick in the number of cases with respect to [hospital] admissions, but in Trivandrum, in fact, there's a down[ward] shift in the number of cases. So it's a mixed spread here. But I can assure you that over the next two or three weeks, once the festival season kicks in, we can expect a greater number of cases and I'm concerned about that.
Dr Ramankutty, how do you see Kerala's increasing Covid-19 cases from your perspective as an epidemiologist? Why is this happening and where could it go?
VR: First of all, let me be very frank, I have no final answers. We can only go by what is reported to give you some plausible explanations. But they are just plausible explanations. First of all, [Kerala's increase in cases] is based on reporting, and the quality of reporting may vary across states--that is something you have to recognise. But let us discount that phenomenon. I do think that Kerala has [a high] number of Covid-19 cases, no doubt about it. But is it so alarming? If you ask me, not yet, because as Dr Rajeev pointed out, we have not come to a situation where the hospitals are overwhelmed and we can't cater to people who need healthcare.
That, however, doesn't mean that we can be less vigilant. Again, as he pointed out, the festival season is coming, there are a lot of people who are still not vaccinated or have [not] got the disease in the state. That means there are a lot of vulnerable people and Covid-19 numbers can go up. Right now, the fact that cases are not really being controlled as we expected is definitely a downside and we have to look at the reasons for that. I think part of the reason is that there were occasions in between when--even though there was a lockdown--people were out in the streets, you could see a lot of crowding in many places. I don't know, but perhaps that has led to the situation where [case numbers] are not going down. So that's all I can say now. I really don't know the answers.
But if you were to look at the number of Covid-19 cases and testing in Kerala versus other states, let's say states where potentially there could be movement of people and thus transmission, what are Kerala's numbers telling you?
VR: As you said, almost one-third to half of all Covid-19 cases being reported every day in India are from Kerala. Many districts are reporting 1,000-2,000 cases a day, which is not a very happy situation. So altogether, currently statewide there are about 20,000 cases being reported, which is much greater than all the other states. This is really troubling and we have to find an explanation. I really don't know why it is so. It could be the way people are behaving in the state, but this is a state where most of the Covid-19 instructions--at least in my observation--have been more or less followed. I don't see many people without masks in Kerala. The only troubling thing I find is that there's certainly some crowding in the shopping centres and other places where people gather. So that probably is [the reason why], but then there is a trade-off between how much you can control people because there's a lot of economic hardship due to the lockdowns.
Dr Jayadevan, you mentioned a downshift in Covid-19 cases in Trivandrum and a slight rise in Kochi. Tell us about the nature of the cases themselves. Are they exhibiting the same characteristics of the Delta variant? Are you seeing any changes in the manner in which Covid-19 is being transmitted in Kerala? You mentioned transmission is happening within homes. Is that a course which is different from earlier? Or is there something fundamental which may not have changed, that's retriggering the spread?
RJ: I was asking the same question to a group of doctors online yesterday. I'll tell you the highlights. The first is that the incubation period-which is basically if I get the virus today, when do I get fever--has come down to less than two days, in many cases. And that's confirmed. This used to be five to seven days last year. So with the new variant and whatever changes have been happening in the environment and our immune system, incubation is shortened. So it's becoming incredibly hard to isolate these people. How do you isolate someone when the virus is spreading practically in less than two days?
The second is that fully vaccinated people are picking up the virus. I use the words 'picking up' very specifically here, because they're not getting sick. They're picking up the virus and importantly, they're spreading the virus as well. Because a good majority of them are not adept at immunology or epidemiology, they believe that if they are vaccinated, they can't pick up the virus and I don't blame them for that.
If you notice over the last year, the narrative has been 'if you're vaccinated, that's a miracle'. The Western media have used superlative words like 'miracle'. There's no miracle here. Vaccines are a product that decreases your risk of dying if you pick up an infection. That's the long and short of it. But this has been played up by international media and vaccination campaigns saying that [the vaccinated] are totally bulletproof. No, that's not true. People are picking up the virus in the throat and nose and unfortunately, they have dropped their guard and they are mingling like they would not have the virus. If you believe that you are immune to the virus, imagine what damage you could do to your family, your workplace and your social circle. And you multiply that with the millions of people who have received vaccines. So that is a risk factor that needs to be immediately addressed, not just in India, but across the world.
Whispers have begun. Loud whispers are coming from the US. The CDC [Centers for Disease Control and Prevention] announcement and the document that they have under consideration right now, contains alarming information. That is point two, that vaccinated people can't drop their guard, they have to take the same precautions as everyone else. There's no need to be alarmed, you won't die. But if you've been vaccinated, you could be carrying the virus home and elsewhere.
There's no change in the disease pattern. The way the human body responds is the same. There is no shift in the age group, either. It's pretty much the same age group and same male-female ratio. We look very closely at things like the hospitalisation pattern. Over the last month or so, the kind of patients that have come in are not the sickest, as we saw in the beginning of the [second] wave in April-May all over India. This time, over the last month or so, we've not had such sick patients coming in.
Dr Ramankutty, when you look at the phenomenon of the spread of Covid-19 in Kerala, explainable or not, how do you extrapolate this to what is happening or not happening in the rest of the country?
VR: There are some indications from the seroprevalence studies that actually the proportionally infected people is higher in many other states, because probably [more people] got infected, and because their vaccination coverage is not so high. This means that the proportion of people who are vulnerable is low, but if there is a variant, then this doesn't really mean anything, so [the virus] can actually [make] a comeback. To the extent that the same virus is spreading, that bodes well for states where the proportion of people who are vulnerable will be low.
In fact, in Kerala, one of the explanations that people have put forward is that we have a low seroprevalence, because we have done the protection right, post the first [wave], so we'll have more vulnerable people for the second [wave]. It is like a second generation problem, which you always find in Kerala. Generally, the public health people say that we have brought down death rates in Kerala, thus there are a lot of old people, so that is another problem. These are called the second generation issues. [The current spread] might be a second generation issue in Kerala also [right now], I wouldn't rule it out. But the seroprevalence studies are random. The state has done its own study. Sample sizes [aren't] planned in such a way that you can extrapolate it to the whole country, and you're really reading too much into some of those numbers. But still, it does tell you something that many other states have a high proportion of people with antibodies in the first place.
The figures are 68% for the rest of India and about 43% for Kerala. Dr Jayadevan, what does this say about the way the Covid-19 virus will remain around us? Because a certain number of people are exposed at one point, then the virus leaves and comes back, and then another set gets exposed. As the numbers of people who've been exposed are low, the potential of more and more groups of people getting exposed over time remains high. Is that a correct presumption?
RJ: That is partly true; I'll explain. The first thing to understand is that the spread of a pandemic in a region is stochastic. That's the technical term. 'Stochastic' is best explained by looking at a slice of bread and seeing how mould appears. Mould doesn't appear in every part of the slice at once. It appears in one part, then another, and another, and so on. There are many reasons for this. We have a habit of putting things in boxes, organising things, naming and classifying them. That's good to some extent, but you can't classify things beyond an extent.
For example, if you look at the US now, the southern states of Florida, Texas and Louisiana are seeing several Covid-19 cases. Now, if you forget the state names and just look at the south-west coastal and northeastern states in India and then at the neighbouring island of Sri Lanka, which is also affected, you'll see there's a pattern. If you look at the weather patterns in these areas, these have the maximum relative humidity, which is basically the amount of water vapour that is hanging in the air at any given point in time. This is a complex topic, I'm not pretending to conduct a physics class. But basically, there are factors beyond what we know here.
For instance, if I am a Covid-19 patient and if I am to transmit my virus to someone else, the virus has to travel through the air. There are factors that determine how efficiently I can transmit this virus to the next person. That is determined by temperature, relative humidity, wind speed, crowding, ventilation, and so on. There are two key factors that determine how efficiently I transmit my infection to someone else: A, my behaviour, i.e. if I take off my mask, if I'm careless, I laugh and talk in a closed room with a bunch of people, I can transmit the virus. B, if the virus itself is able to stay alive inside the droplet for a longer period of time, and also if the droplet that is carrying the virus survives in the air for a longer period of time.
These are extremely complex topics, from papers published on fluid dynamics, so they're really not good for mainstream discussion but your questions are so precise, I thought I had to throw in this variable, which I believe is profoundly important. Florida and Texas have the highest relative humidity and the highest dew point in the whole of America. Obviously, there's a lot of political blame factor that is built into the pandemic. Let's forget the political part of it. But clearly, there are these factors that affect the spread of the virus in the air. It's an airborne virus. A virus doesn't walk or fly, it has to catch a vehicle. How effectively does the virus stay alive till its destination? These are factors that we looked at.
Dr Ramankutty, assuming the transmission of Covid-19 continues at the pace that it is today, going by the fact that we are seeing these surges in the western coastal states, how is the life cycle of the pandemic in India looking to you, as you look ahead?
VR: I wouldn't like to make any predictions but we always have to assume that the worst will happen. You have to be prepared for another wave, especially in terms of hospital beds and care facilities. We should not be caught off guard if there is another wave.
I think what Dr Rajeev has said has a lot of interesting aspects. We didn't know much about how the virus spreads, initially. There were a lot of theories about touching surfaces and fomites, etc. There are physicists who have studied how the virus stays airborne and they have come up with some interesting theories, especially from Britain. I have read some interesting theories where they have specified how many people can sit in what size of room. Just like the weather, local conditions mean so much for the spread of Covid-19, and probably that is why we are seeing different patterns. I think this hypothesis is very interesting and should be probed.
That brings me to another point. In India for some reason, unfortunately, though we have large research manpower, they have not been encouraged to study this. It's very secretive and nobody lets you do anything unless you have the government imprimatur. That has really held us back. We should have studied the processes and come out with more understanding of how the Covid-19 pandemic is shaping up in India, especially with the variants. I think we have failed to do that. It's a big failure, one of our cardinal sins.
Dr Jayadevan, let me come back to Kerala. The state has a high number of Covid-19 cases but hospital bed occupancy is under control. At this point, with the second wave ebbing in many parts of India but a possible third wave beckoning, what is it that concerns you most? And what is it that you're more optimistic about?
RJ: What concerns me most is the festival of Onam, which is not a religious festival. It's really a harvest festival that's pretty much like Christmas of the West for Kerala, when most traders make a year's worth of earnings. So, Onam is big. On the one hand, we need to have people make their livelihoods. And doctors, including us, who frequently speak and write about Covid-19, have always stood with the common man, for them to be able to open their stores, go to work, make their sales, and so on. So we need to make that happen. And at the same time, we have to make sure that the process of making that happen does not put the community at risk. Now, that's a fine line.
I went through the latest state government guidelines, and it is pretty encouraging. The 20-point annexure from the government of Kerala is very impressive. It took into account the fact that we talked about the aerosol spread within a room. They talked specifically about the 25-square-foot space per person, and I was hugely impressed with that, because I was always advocating for schools to consult architects and engineers to improve their ventilation systems. Remember, for any given room, there is x cubic feet of air and there's an air replacement rate. So if you keep the room completely closed, there is no air replacement at all and so your risk [of Covid-19 spreading] is very high. But if your H-VAC system has a good air replacement rate, your risk is low. That's what Germany and other nations have tried to achieve over the last year. We need to think in that direction.
Secondly, you rightly pointed out that we need to rely more on local indices. I'll give you an example. Kerala's curve has been different from the beginning of the pandemic. Kerala had a big peak last Onam, which is why I'm concerned now. And the second peak occurred, believe it or not, in January. At these Tuesday meetings that we hold here, we picked that up very early. We found out that there was an uptick in ICU admissions right through January and we put out a major press release warning the government, saying the ICUs are filling up, be careful. And the government immediately responded with firm measures and the ICU occupancy rate came down to 30%.
So my point here is in the long run, every region will have to look at how much of their facilities are being used up. Don't wait until you're full. You've got to act when you're about halfway full because this thing is like a train, it doesn't stop like a car. You put the brakes in the form of whatever restrictions, it'll take about a month to show the effect.
Anything more that you can add to the point you had made earlier about rapid incubation?
RJ: See, the virus is able to efficiently enter our body, that is the reason why the incubation period is shorter. And that is because the virus has adapted its receptor-binding protein to attach more efficiently to our ACE2 receptor. Basically, it is the spikes of the virus that attach more efficiently to our system. There's a way in which it cleaves its spike protein; the molecule is split in two [as if] by a pair of scissors and it uses it as a hair clip to enter and fuse with the cell membrane. I know that's technical jargon but I want all to know that the virus is very smart. So that explains why the incubation period is shorter.
What we need to do, looking forward, is to communicate this effectively. Communication is an important part of [controlling] the pandemic and that is one area where Kerala stood out. Doctors were constantly on the media, the media were with the doctors, the chief minister would speak every day. And there were programmes on the radio. So the communication was very good, and that's very important. It's not about vaccination or mutations; basically, it's communication.
So I think that the factor that I mentioned here, that vaccinated people are picking up infections, must be communicated very delicately to the public, because it can turn around on itself. People might just stand up and say, 'Look, you guys were telling us that vaccines are good'. Remember, people love either black or white. Either it works or does not work, there's no in-between. So we have to be very careful how we communicate this to the public, because we don't want to push vaccine hesitancy. Vaccine hesitancy is lowest in Kerala and that's the combined effort of a lot of people. That's really a triumph of communication. But we need to be very delicate in the way we communicate this.
Dr Ramankutty, what is something that you're concerned about and something you're optimistic about?
VR: From Kerala's standpoint, Onam is a big concern, because people want to celebrate. Onam is the time when families and friends get together, buy things, go out shopping. So they are looking forward to all this and the government certainly will be forced to at least give some concessions on that front. And as a doctor, even though I fear what might happen, I would certainly not say that the situation is so bad that you have to keep to your houses. No. We have to allow this but do it in a controlled fashion, as well as expect something might go wrong at some point and then be prepared for that. So that is a big concern.
Secondly, it is a good thing that Kerala has the highest proportion of vaccinated people and we have to push this. There are concerns about that. People have been saying that it's more difficult to get vaccinated in Kerala compared to other states. I don't know how far that is true but if it is true, the government certainly has to correct that. But that vaccinated people can spread the disease, that is a message where again, we have to be very careful. You cannot frighten people off vaccination, but we have to tell them in the correct language that even though you're vaccinated, you still need to mask and not go out in crowds and keep all those social distancing norms, to the extent which is mandated.
The plus point is the rising level of vaccination. People looking forward to getting vaccinated is something that I think is unique to Kerala. I don't see much vaccine hesitancy here. That's a good thing.
We welcome feedback. Please write to respond@indiaspend.org. We reserve the right to edit responses for language and grammar.


